What Are The Causes Of Persistent Itchy Skin In Seniors Without A Rash?
Outline and Reading Guide: Why “Itchy Skin, No Rash” Matters in Later Life
When itch strikes without a visible rash, the uncertainty can be as irritating as the symptom itself. For many older adults, persistent itch—also called pruritus—springs from a mix of age-related skin changes, environmental triggers, medications, and sometimes deeper medical issues. A clear roadmap helps cut through the noise and directs attention to steps that actually make a difference. This guide starts with an outline so you know exactly what to expect, then walks you through causes, treatments tailored to seniors, and how to find a skin and allergy clinic near you if you need specialized care.
Here’s how we’ll navigate the topic:
– Section 1 (you’re here): Why the subject matters, how the article is structured, and what outcomes to aim for, such as restful sleep and safer skin care routines.
– Section 2: Itchy skin in seniors with no rash—common causes, from dry skin to neuropathic signals and systemic conditions, plus what warning signs to watch for.
– Section 3: Evidence‑based treatments for older adults, including moisturizing strategies, topical options, medications to discuss with your clinician, and light therapy.
– Section 4: Practical steps to locate a nearby skin and allergy clinic, what to bring to the appointment, and questions that help you get clear answers.
– Section 5: Day‑to‑day prevention, home adjustments, and caregiver tips to reduce flare‑ups and support long‑term comfort.
Why focus on seniors? With aging, the skin’s barrier thins and natural oils decline, making dryness and itch more likely. Nerve changes can amplify itch signals, while long medication lists and chronic conditions add layers of complexity. Surveys in temperate climates consistently find that older adults report dry, itchy skin more often in colder months, and clinicians see non‑rash itch as a frequent reason for visits. While exact numbers vary across studies and regions, the burden is clearly significant—and the solutions are rarely one‑size‑fits‑all.
What outcomes are realistic? Relief is often cumulative: small, consistent steps typically beat quick fixes. In many cases, gentle bathing habits, strategic moisturizers, and smart wardrobe choices reduce symptoms substantially. For itch driven by underlying health issues, treating the root cause is key. And when home measures fall short, collaboration with a dermatologist or allergy specialist can uncover targeted therapies. Keep a curious, steady approach; the goal is progress, not perfection.
Itchy Skin in Seniors Without a Rash: Common Causes and How They Work
“Itchy skin, no rash” often points to mechanisms that don’t always show on the surface. In later life, the most frequent driver is xerosis—very dry skin. With age, the outer barrier loses lipids and natural moisturizing factors; sweat and sebum production fall; and the skin’s acidity can shift, all of which weaken the shield that keeps moisture in and irritants out. The result is a sensation of itch long before redness or visible scaling appears. Cooler, drier seasons intensify this effect, as indoor heating lowers humidity.
Beyond dryness, several pathways deserve attention:
– Neuropathic itch: Conditions that affect small nerve fibers (for example, long‑standing diabetes or spinal nerve compression) can trigger itch signals without surface changes. People sometimes describe “pins and needles,” burning, or localized hotspots (like notalgia paresthetica between the shoulder blades).
– Systemic causes: Internal conditions—including thyroid imbalance, iron deficiency, kidney disease, and liver or bile flow disorders—may present as generalized itch. In cholestatic states, bile salts and other mediators can stimulate itch receptors; in advanced kidney disease, metabolic byproducts may play a role.
– Hematologic and malignancy‑related itch: Certain blood disorders and some cancers can cause persistent, unexplained pruritus. While uncommon, this is why unexplained, worsening itch with other symptoms merits prompt evaluation.
– Medication‑related itch: Opioids, some blood pressure medicines, diuretics, and other drugs may provoke itch directly or by drying the skin. Adjustments should only be made with your prescriber’s guidance.
– Psychogenic contributors: Anxiety, stress, and disrupted sleep can magnify itch perception, creating a cycle where scratching begets more itch.
Red flags that deserve timely medical assessment include: itch lasting more than six weeks without clear triggers; B‑symptoms like unintended weight loss, night sweats, or persistent fever; jaundice or dark urine; severe sleep disruption; and any new medication started shortly before the itch began. In older adults, multiple mild factors frequently stack together—slightly dry air, a wool sweater, a long shower, a new pill—until the brain’s itch threshold is crossed. Think of it like a bucket: single drops may be harmless, but enough of them overflow into constant discomfort.
For context, clinicians often see seasonal spikes in winter and in regions with low ambient humidity. Studies differ on exact prevalence, but many report double‑digit rates of chronic pruritus among older populations. The key takeaway: a methodical check of skin care habits, wardrobe, home humidity, medications, and medical history usually reveals modifiable levers—no rash required.
Elderly Itchy Skin Treatment: A Stepwise, Senior‑Friendly Approach
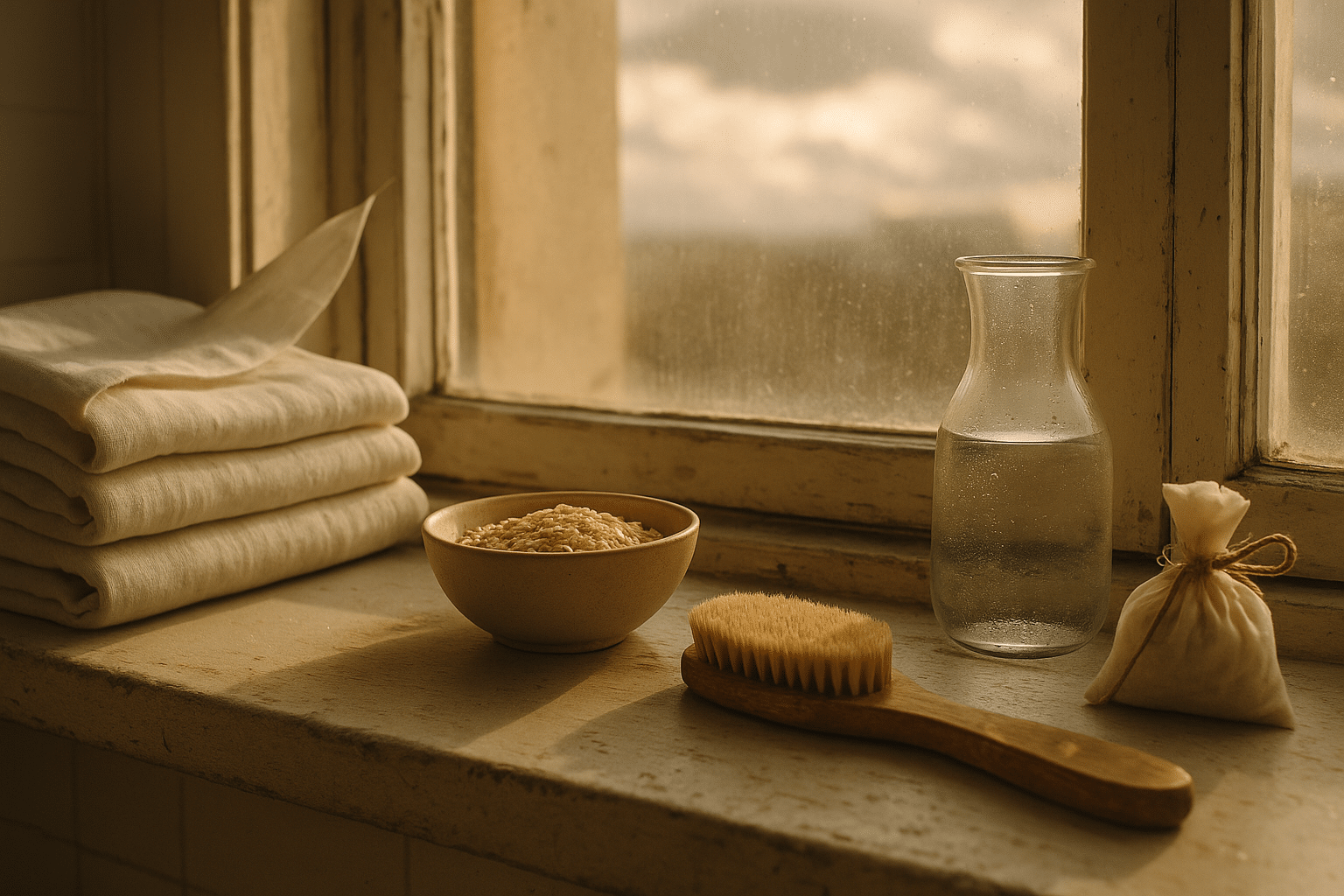
Effective relief usually starts with the skin barrier. Aim to lower the skin’s “itch noise” so nerves fire less often and healing accelerates. Begin with bathing and moisturizing: choose short, lukewarm showers or sponge baths; use gentle, fragrance‑free cleansers sparingly; and apply a rich, occlusive moisturizer within three minutes of toweling off. Ingredients often favored for senior skin include ceramides, glycerin, petrolatum, shea butter, urea (for very dry, scaly areas), and lactic acid at low concentrations. Patch test new products on a small area first to avoid surprises.
Daily routine tips that make outsized differences:
– Moisturize twice daily on arms, legs, and trunk; increase frequency during cold, dry months.
– Keep fingernails short and smooth; consider cotton gloves at night to curb unconscious scratching.
– Choose soft, breathable fabrics like cotton or bamboo; avoid wool and rough synthetics against the skin.
– Run a room humidifier in winter and target indoor humidity around 40–50%.
– Use cool compresses for sudden hotspots; avoid very hot showers, which strip oils.
Topical therapies can add targeted relief. For non‑rash pruritus, lotions with menthol or pramoxine can soften itch perception. Capsaicin cream may help localized neuropathic areas after a careful, gradual introduction (initial warmth is common). When low‑grade inflammation is suspected, non‑steroidal immunomodulating creams or mild topical steroids may be considered for short courses under clinician guidance. Be cautious with frequent or long‑term steroid use on thin senior skin.
Oral options depend on the mechanism. Non‑sedating antihistamines have limited value for non‑histamine itch but may help when allergies are involved; sedating antihistamines can aid sleep but must be used judiciously in older adults because of fall risk and next‑day grogginess. For neuropathic drivers, medications that calm misfiring nerves—such as certain gabapentinoids—may be appropriate at low, slow‑titrated doses. In cholestatic itch, bile‑acid binding agents or other targeted therapies may be discussed with specialists. Phototherapy (narrowband UVB) is a well‑established, clinic‑based option for stubborn, generalized itch, particularly when systemic causes are ruled out or treated.
Two practical notes: first, simplify. Many seniors see more relief from consistent basics than from juggling five creams. Second, track patterns. A small notebook or phone log that records itch intensity, sleep quality, weather, meals, and medications can reveal triggers or timing that aren’t obvious day to day. With persistence, most people build a toolkit that meaningfully reduces symptoms and restores comfort.
Skin and Allergy Clinic Near Me: How to Find the Right Local Expertise
When home care and primary visits aren’t enough, a focused evaluation can save time and guesswork. The challenge is translating “skin and allergy clinic near me” into an appointment that answers the right questions. Start by searching for dermatology and allergy practices within reasonable travel distance, then refine the list with a few quality checks that don’t require insider knowledge.
Smart ways to narrow options:
– Confirm clinician credentials and experience with pruritus in older adults; look for profiles that mention chronic itch, geriatric dermatology, or patch testing.
– Review clinic services: patch testing for contact allergens, skin prick testing for inhalant or food sensitivities, phototherapy availability, and access to on‑site lab draws can streamline your work‑up.
– Scan independent patient feedback for comments about clear communication, punctuality, and careful follow‑up (focus on patterns, not one‑off opinions).
– Check practicalities: wheelchair access, parking, public transit proximity, and whether the clinic is in‑network for your insurance.
– Call the front desk with two or three focused questions to gauge responsiveness and clarity.
Prepare for your appointment so the visit delivers maximum value:
– Bring a complete medication and supplement list, including start dates.
– Pack your current skin and laundry products or photos of ingredient lists.
– Keep a two‑week symptom diary noting itch severity (0–10), sleep disruptions, clothing worn, bathing habits, and any new exposures.
– Note systemic symptoms: fatigue, weight shifts, sweats, jaundice, or changes in urine or stool color.
Good questions to ask include: What are the leading possibilities for my itch if there’s no rash? Which tests, if any, can narrow the cause? How do we prioritize treatments with my other conditions and medications? What’s a realistic timeline to judge whether a therapy helps? Are there lifestyle changes that might give me quick relief while we investigate deeper causes?
Red flags to avoid: clinics that promise overnight cures; pressure to buy expensive product bundles on the spot; or a reluctance to review your medication list and general health. A well‑regarded clinic will welcome your notes, explain trade‑offs, and outline a staged plan so you leave with next steps rather than more uncertainty.
Prevention, Daily Routines, and Caregiver Tips for Long‑Term Comfort
Sustainable relief comes from routines that are easy to keep even on busy days. Think of your skin like a house: first, weatherproof the outside; second, control the indoor climate; third, reduce sparks that could start a fire. That translates to moisturizers that seal in water, steady humidity indoors, calm fabrics against the skin, and habits that interrupt the itch‑scratch cycle.
Core daily habits that pay off over time:
– Set a “moisture alarm” after bathing and before bed; moisturize generously on limbs and trunk.
– Keep showers brief and lukewarm; swap foamy washes for mild cleansers on the groin, armpits, and feet only, and simply rinse elsewhere.
– Rotate two or three comfortable outfits made of breathable fibers; launder with fragrance‑free detergents and skip fabric softeners if they seem irritating.
– Use a hygrometer to keep indoor humidity near 40–50%; too low dries skin, too high can encourage dust mites and mold.
– Create a bedtime wind‑down: cool room, light blanket, fan or white noise, and a no‑scratch rule supported by cotton gloves if needed.
Nutritional and wellness touches matter as well. Adequate hydration supports skin turgor; consistent protein intake helps repair; and varied fruits, vegetables, and healthy fats nourish the barrier. Evidence for supplements is mixed, so consult your clinician before adding anything new, especially if you take multiple medications. Gentle movement, breathing exercises, or short walks can reduce stress‑related itch amplification, and brief mindfulness practices at bedtime may improve sleep continuity.
Caregivers play a pivotal role. Help with moisturizer application to hard‑to‑reach areas; label morning and evening routines on a simple checklist; and watch for changes that suggest new triggers, such as a recently opened lotion or a different laundry product. If memory issues are present, keep products in one basket with large, color‑coded caps to reduce confusion. Track any skin breaks or bruises, since older skin is fragile; prompt care for scratches prevents secondary irritation or infection.
Finally, revisit the plan every few weeks. If itch severity plateaus above your comfort level, or new systemic symptoms arise, circle back to your clinician. Most seniors find that a steady, layered approach—barrier care, environment tweaks, smart fabrics, and targeted therapies—gradually turns down the volume on itch, leading to quieter nights and more comfortable days.


